Written By: Maureen Testoni President & CEO 340B Health
Maureen Testoni is the president and CEO of 340B Health, which represents more than 1,400 hospitals participating in the 340B drug pricing program
This year marked an important milestone for the 340B drug pricing program. On November 4th, we celebrated the 30th anniversary of 340B. In the three decades since President George H.W. Bush signed it into law, 340B has enabled nonprofit hospitals, health centers, and clinics to serve communities in every corner of our country. Thanks to 340B, patients receive quality care closer to their homes, jobs, and families. Communities have access to vital health services and delivery networks needed to sustain a robust social fabric. And all this has been possible because of a program that has enjoyed bipartisan support across five administrations, 15 Congresses, thousands of communities, and millions of Americans without relying on taxpayer dollars to fund the care.
Despite these successes, the stakes have never been higher for those of us who advocate on behalf of 340B and the providers who participate in it. With 340B growing and evolving to meet changing patient health needs, it has gained more national attention than ever before. Ten years ago, we might have had trouble finding people who had even heard of 340B, let alone who were familiar with the critical role it plays in bolstering the health care safety net. Now 340B is appearing regularly in publications throughout the U.S., in the floor speeches of prominent members of Congress, and even in the highest court in the land.
With that increased attention has come increased challenges for 340B covered entities and their patients. We have had to defend 340B on several new fronts that never were in play before.
340B Health, which represents more than 1,400 health systems and hospitals, advocates on behalf of 340B. We also work to help our member pharmacists, 340B program managers, and other health professionals run effective, compliant programs for the benefit of patients in need. As we wrap up the 30th anniversary year for 340B, we are centered on several key trends and areas of focus that we believe will be pivotal for the future of the program.
Drug Industry Attacks on 340B
The pharmaceutical industry recently has been pushing hard to change the program in ways that diminish the amount of help it provides to safety-net providers and the patients with low incomes whom they serve. This is not true for all drug companies, as more than 700 participate in 340B and continue to abide by the law.
Since 2020, the single biggest challenge to 340B has come in the form of pharmaceutical company restrictions on savings for covered entities. After years of unsuccessful attempts to convince Congress to make cuts to 340B, several major drugmakers started unilaterally restricting discounts to covered entities on drugs dispensed at community and specialty pharmacy partners, actions that the Department of Health and Human Services (HHS) has said are illegal.
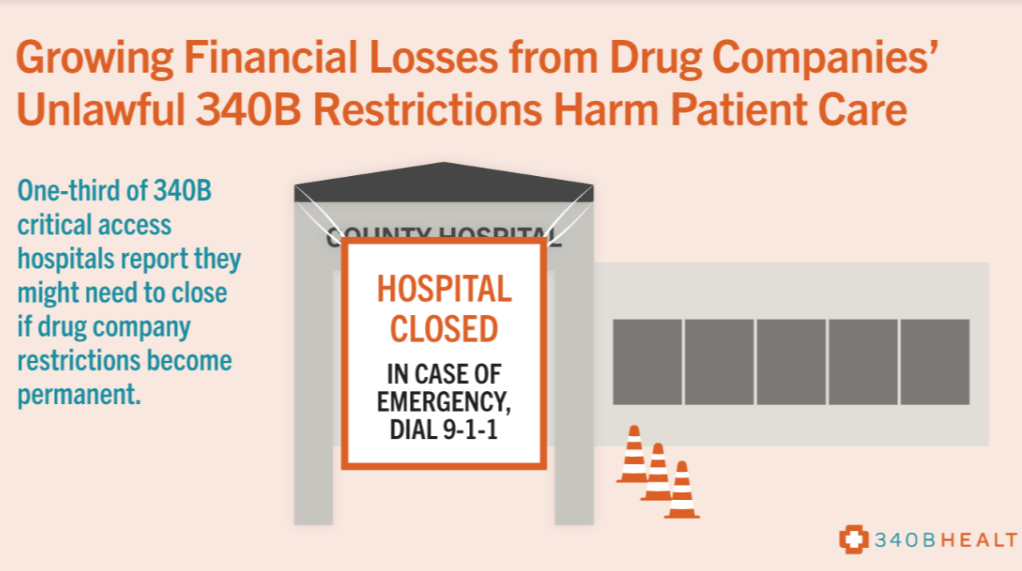
What started with a handful of companies has now expanded into a major threat to 340B. The companies now restricting access to 340B discounts include several of the largest drugmakers in the world that collectively brought in more than $600 billion in revenues in 2021. Their actions have caused immense harm to safety-net providers who rely on these savings to treat their patients in need. A survey of hospitals we conducted in early 2022 found larger, typically urban 340B hospitals reporting average financial losses of millions of dollars per year because of these restrictions. Smaller, typically more rural hospitals are losing hundreds of thousands of dollars per year on average. These losses are devastating to facilities that already rely on the thinnest of operating margins to stay open.
Why are these drug companies waging this assault on 340B savings? Not surprisingly, the answer is rooted in a systematic pursuit of profits. Our analysis of the companies that are restricting access to discounts and the drugs they are targeting for these restrictions demonstrate two main strategies companies are using to boost revenues at the expense of safety-net providers and patients. The first focuses on denying access to discounts for some of the costliest specialty drugs that physicians are prescribing for patients living with chronic diseases, including various forms of cancer. The second focuses on getting around the federal penalties imposed on them after they raised the price of drugs much faster than the rate of inflation. For such drugs as insulin, for which the price skyrocketed 1,200% over the past two decades, these penalties permit 340B providers to pay a nominal amount and use the savings to care for more patients.
The unilateral cuts to 340B from these manufacturers keep more dollars in drug company coffers and deprive safety-net hospitals of resources they need to fund patient care. Both the Trump and Biden administrations have told the drugmakers they are breaking the law. But instead of complying, several companies went to court to challenge the government’s authority. Several federal appeals courts heard oral arguments in those cases earlier this fall as part of what we expect to be a protracted legal battle over the drug company actions.
In the meantime, pharmacists and other health providers are continuing to do their utmost to preserve 340B-funded care for patients in need amid the cuts in savings. Many of these providers also are sharing the challenges of doing so with lawmakers, media outlets, and others. Complaints and reports against 340B restrictions have led to bipartisan shows of support for covered entities from members of Congress and state elected officials. It has aided immensely in the federal government’s efforts to pursue strong enforcement actions against the companies and to assert its authority to do so in federal courts. And it has put the drug industry in the position of defending the reputations of companies that are harming the health care safety net by cutting 340B.

The End of Medicare 340B Cuts
The federal litigation process can take a significant amount of time to navigate, and it can have mixed outcomes for the parties involved. But a years-long legal battle over Medicare payment cuts to 340B hospitals recently culminated in a decisive victory for the hospitals.
Starting in 2018, Medicare started cutting its payment rates for outpatient drugs used at most 340B hospitals. A group of hospitals and hospital associations filed a lawsuit against the government challenging the pay cuts. Hospitals said the cuts forced them either to offer fewer comprehensive services to patients in need or to postpone planned expansions of that care.
It is rare for a lawsuit to make its way to the U.S. Supreme Court, and it is rarer still for a case to result in a unanimous decision. But earlier this year, all nine justices signed onto a decision stating that Medicare broke the law when it applied the cuts just to 340B hospitals without first conducting a required survey of hospital drug acquisition costs. The high court sent the issue back to a lower court to determine what remedies affected hospitals should receive for the years’ worth of unlawful cuts.
The Supreme Court decision resulted in some long-overdue clarity for 340B hospitals about how much the law requires Medicare to pay them for outpatient drugs that they prescribe But that development did not settle the question of how 340B hospitals would be made whole for the nearly five years’ worth of cuts that they have sustained under the unlawful policy.
Federal officials and courts will continue to work out the remedy details, a process that we expect could take a significant amount of time to complete. We have told the government that affected hospitals should receive repayments to cover the full amounts for outpatient drugs that they should have received had Medicare set the rates correctly since 2018, plus interest. We are opposing any future attempts to implement new drug payment cuts based on hospital drug acquisition cost data, as this would bring back cuts that are antithetical to the intended 340B benefit for the health care safety net.
The Supreme Court decision remains an important victory for 340B hospitals that goes well beyond Medicare. Private health insurers and pharmacy benefit managers (PBMs) had cited the Medicare policy as a precedent for imposing their own payment cuts on providers purchasing 340B drugs at discounted rates. The unanimous decision eliminates that precedent and makes it much more difficult for payers and PBMs to justify their discriminatory payment rates for covered entities.
Heightened State Activity on 340B
The importance of 340B also has drawn the attention of state officials. Much of the recent attention in the states has focused on the same type of payment discrimination that was at play in the federal court fight over Medicare payments.
Increasing numbers of states have been cracking down on discriminatory payment policies by health insurers and PBMs that effectively divert the benefit of 340B from the providers for whom it is intended. Before 2019,no state had a law banning 340B payment discrimination. Now nearly half of the states in the U.S. have such statutes on the books, and that number continues to grow every year.
These laws vary in terms of what types of discriminatory payment they ban and what covered entities they protect. The typical statute bans payers and PBMs from paying less for a 340B-purchased drug than they pay a non-340B provider for the same drug or from assessing additional fees or chargebacks on providers just because they participate in 340B. Several states ban burdensome claims reporting requirements on covered entities that do not apply to other providers. Some have extended the scope even further than private insurers and PBMs to prohibit drug companies from refusing discounts on drugs dispensed at contract pharmacies, though those protections are facing legal challenges. To assist states considering adding such protections, we have developed model state 340B nondiscrimination legislation for lawmakers to consider.
Looking Forward
All of us in the 340B provider community will continue to track these key trends as we advocate on behalf of the dedicated safety-net health professionals who care for patients in need. 2023 will be bringing more occasions for us to speak out on these topics. A new Congress will mean new opportunities to educate lawmakers on what 340B is and why they should protect it.